The History of Orthodontics
Have you ever wondered or had a patient ask you how orthodontics came to be? Maybe you read through the history of early orthodontists at one point in your career or have always had a personal curiosity about how things like the shape of brackets or the metal used in archwires came to be (did you know that one of the first archwires was actually a piano string?).
Although the most significant changes in orthodontia came in the last 200 years, there are actually over 2,000 years’ worth of history supporting the concern that people and medical providers had for tooth malocclusion.
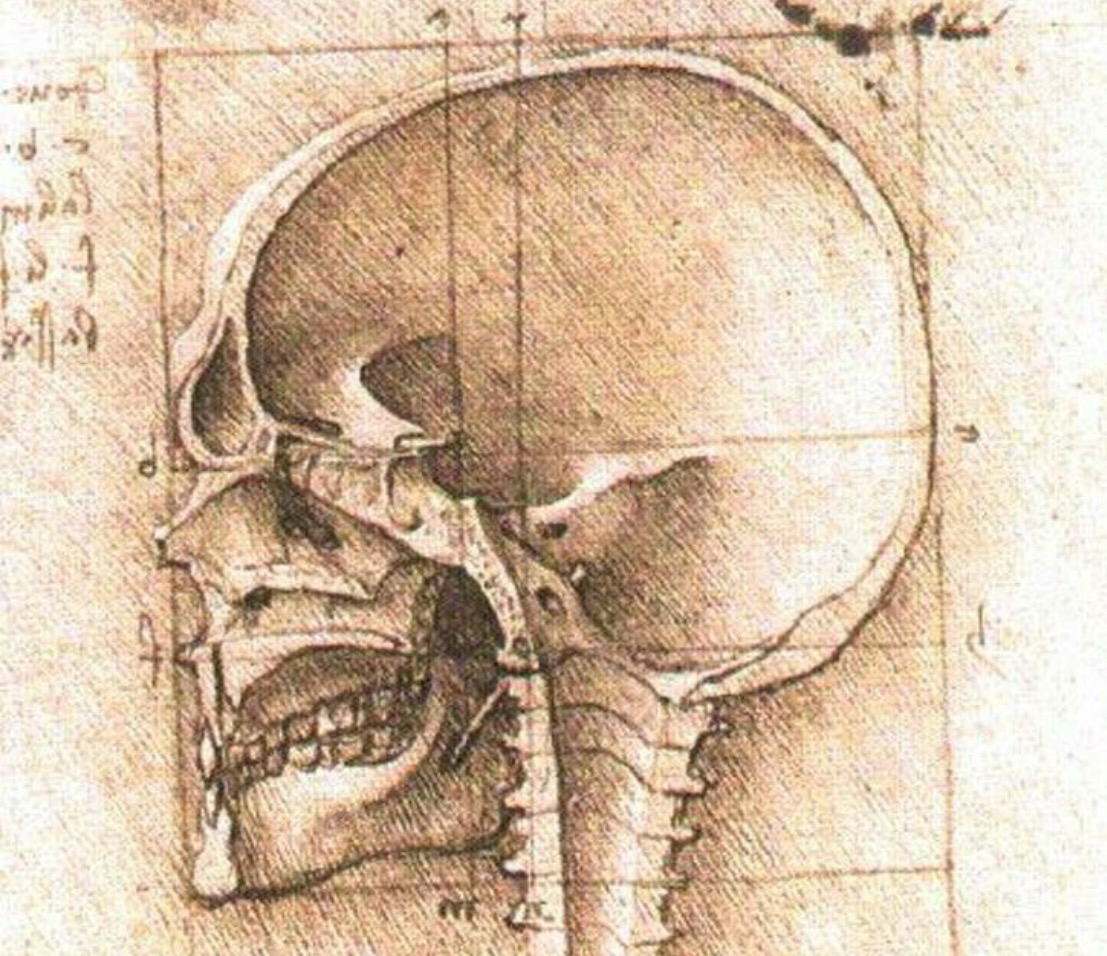
According to the British Orthodontic Society, both Hippocrates and Aristotle (famous Greek physician and philosophers, respectively) described the problems of malocclusion as early as 400 and 350BC. Medical writers a few years later began recommending “treatments” like applying finger pressure or filing down the irregular teeth to address issues such as a lack of space.
The First Orthodontic Device
It wasn’t until the 16th century that human anatomy and medical interests sparked an advancement of knowledge in the treatment of dentofacial problems. By 1728, a French dentist by the name of Pierre Fauchard developed a device used to expand the arches when severe crowding was a concern. The appliance was made from a metallic band that was tied onto the teeth by waxed, silk ligatures. And in 1750, John Hunter is documented to be the first dentist to use a fully metal arch with metal ligatures.
Gradually, other dental practitioners experimented with preventative treatments, extractions of deciduous teeth, and using bite blocks with chin caps to address crossbites.
By the mid 1800s, dentists began understanding how the anatomy and placement of specific teeth played into alignment of the bite, combined with genetic factors and issues such as nursing difficulties during infancy. Types of occlusion were outlined to describe the variations of malocclusion and tooth placement around this time.
But Europeans aren’t the only ones to have incorporated orthodontic techniques or a concern about malocclusion. It turns out that Egyptian mummies have also been found with metal bands around their teeth, implying to archaeologists that an attempt was made to move them while still alive.
Modern Orthodontic Appliances
The first dentist to use screws and elastic bands to rotate teeth was J. M. Alexis Change. Although considered to be the first to use a long-term retention method after treatment, he is especially noted for completing cases in as rapidly as only three months. (Unfortunately, the remodeling process of alveolar bone wasn’t understood until the late 1850s.)
The 1800s held the most significant growth and discovery of orthodontic possibilities and treatment methods. By 1900, Edward H. Angle declared orthodontics as the very first dental specialty. In 1907, the European Orthodontic Society was founded and in 1926 the first international orthodontic conference was hosted in New York. By the 1960s and 70s, specialized programs and post-graduate training for dentists became standard.
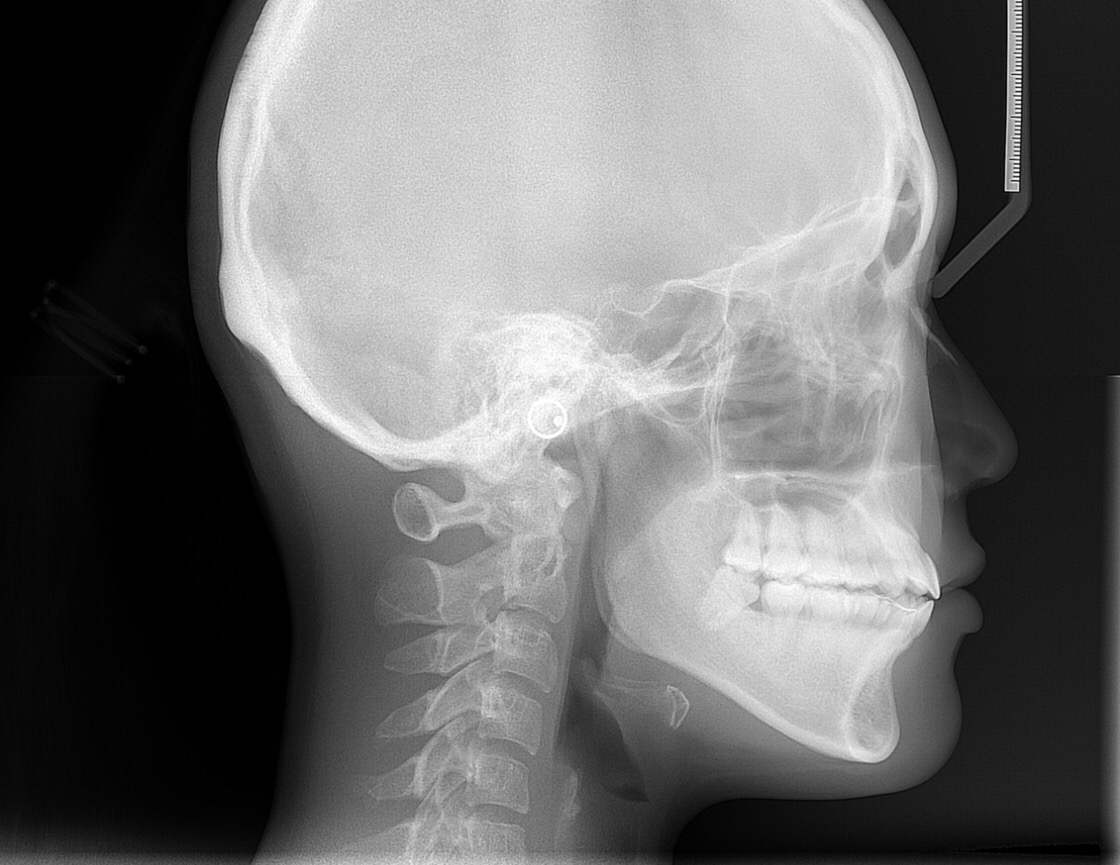
Cephalometrics began to take on a special role in early orthodontics as dentists started to understand the role that teeth played in facial bones and soft tissues. CBCT technology made craniofacial anatomy and tooth positioning easier to assess prior to treatment, allowing orthodontists to opt for plans that would consider specific skeletal abnormalities or surgical procedures as necessary (both for functional and aesthetic purposes.)
Until the 1970s, modern orthodontists attached brackets to metallic bands that wrapped around the teeth. As new materials such as stainless steel began to be incorporated, lingual braces were also introduced.
The Shift from Metal to “Clear” Materials
The early 1980s brought about the invention of the initial type of “clear” or “tooth colored” braces, as ceramic appliances first became available. Some dentists even experimented with removable plastic trays as early as the 1940s. But it wasn’t until 1997 when 3D computer imaging (CAD/CAM) technology made it possible for orthodontic appliances to be crafted in a series of accurately designed removable trays. Invisalign, as it was called, first became available to patients in 2000.
Today, dozens of clear alignment and ceramic orthodontic brands exist. That’s not to mention the other modifications that have been developed over time, such as trap-door systems and changes in the types of metals used for their specific properties.
Although clear aligners were originally most effective for patients who had experienced orthodontic relapse or only faced minor tooth misalignment issues, today’s digital accuracy and treatment planning makes it possible for orthodontists and dentists worldwide to correct a variety of malocclusion and bite cases, including those more moderate to severe.
Digital dentistry and cloud-based treatment planning allows dentists to incorporate the skills of experienced 3rd party practitioners in off-site labs and thus build on the quality of care and types of services available to their patients. As a result, general dentists are also capable of providing limited orthodontics, comprehensive tooth alignment, and even accelerated short term cosmetic braces within their private practices.
Technology that Revolutionizes Orthodontics Around the Globe
As an independent imaging resource, CephX is able to work with a wide variety of the world’s leading orthodontic manufacturers and practitioners to provide cephalometric analysis to provides around the globe.
Do orthodontic scans, CBCT images, X-rays, and other intraoral imaging steps keep your practice from running as efficiently as you would like? Because CephX is fluid with other leading orthodontic support services, we’re able to help you take your dental business above and beyond your current capabilities without the headache of worrying about whether or not your software or imaging tools can integrate with one another.
Thanks to online tracing and automated analysis, CephX clients can access accurate and reliable treatment planning support for their orthodontic patients.
About CephX
At CephX, we provide professionally evaluated orthodontic imaging services to dentists and orthodontists around the globe. Your images are instantly transferred to a secure cloud-based system allowing professionals to resource the support and planning from peers in the field. Not only does this resource improve the quality of care and treatment planning for your existing dental patients, but it boosts the efficiency of your practice and limits out-of-office referrals.
To learn more about CephX, request a free consultation!