Retainers and Maintenance: Preserving Your Patients’ Investment
One of the most overlooked — yet extremely important — stages of orthodontic therapy is that of retention. After all, we all know that relapse is a serious concern for anyone who has recently completed their orthodontic treatment. Yet for many patients, there just isn’t as much concern for a retainer as there is for their braces.
Emphasize Home Care
Your patients remember how important it was to keep their braces, appliances, and other orthodontia completely clean. While they’re still in the same mindset, shift that concern to the maintenance of their retainers before they ever leave your office.
The closer you compare retainers with braces, the easier it is to shift that concern so that they are one and the same. For example, you may want to roll over some of the same “rules,” like:
- Clean your retainer with lukewarm tap water. Hot water could cause removable appliances to warp and not fit properly.
- Use only approved cleansers to lift away debris and prevent buildup, as harsh chemicals could lead to the material becoming brittle, breaking, or discolored.
- Do not eat with your (removable) retainer in place, as it could cause it to break.
- Clean around fixed retainers with the appropriate oral hygiene aids, such as a floss threader or water flosser. Don’t let the patient leave without them first watching and then demonstrating the proper oral hygiene method during their retainer “try-in” appointment.
- Encourage them to see their dentist regularly for preventive care appointments.
- Removable retainers must be worn for a set number of hours per day, or number of days per week, to avoid tooth movement. (Patients with clear removable aligners may relate to this example the most.)
- If something breaks or comes loose, call your office office immediately to have it repaired.
Fixed vs. Removable Retainers
Compliance with any orthodontic treatment is hard. Between removable bands and clear aligners, adding in a removable retainer is just as challenging. There are many benefits to incorporating fixed retainers, especially for patients that may be less likely to comply with wearing a removable device.
However, it’s vital that these individuals have a firm understanding of how to clean areas that are not visible on the facial surfaces of their teeth. Someone who wore lingual braces may be more likely to feel dedicated about flossing under a fixed lingual retainer than, say, someone who wore removable alignment trays.
Removable retainers are still sometimes the best option. When selecting the type of retainer, opting for a clear Essix-type of prosthesis may be better for your adult patients than a Hawley version. When aesthetics is a concern, adults are more likely to better care for their retainer and clean it as advised. Not to mention, many of them like the idea of utilizing their clear retainer as a whitening tray.
More than likely, you’ll know which is the better option for your individual patients based on their past compliance, age, maturity level, and the likelihood of relapse due to their unique anatomy.
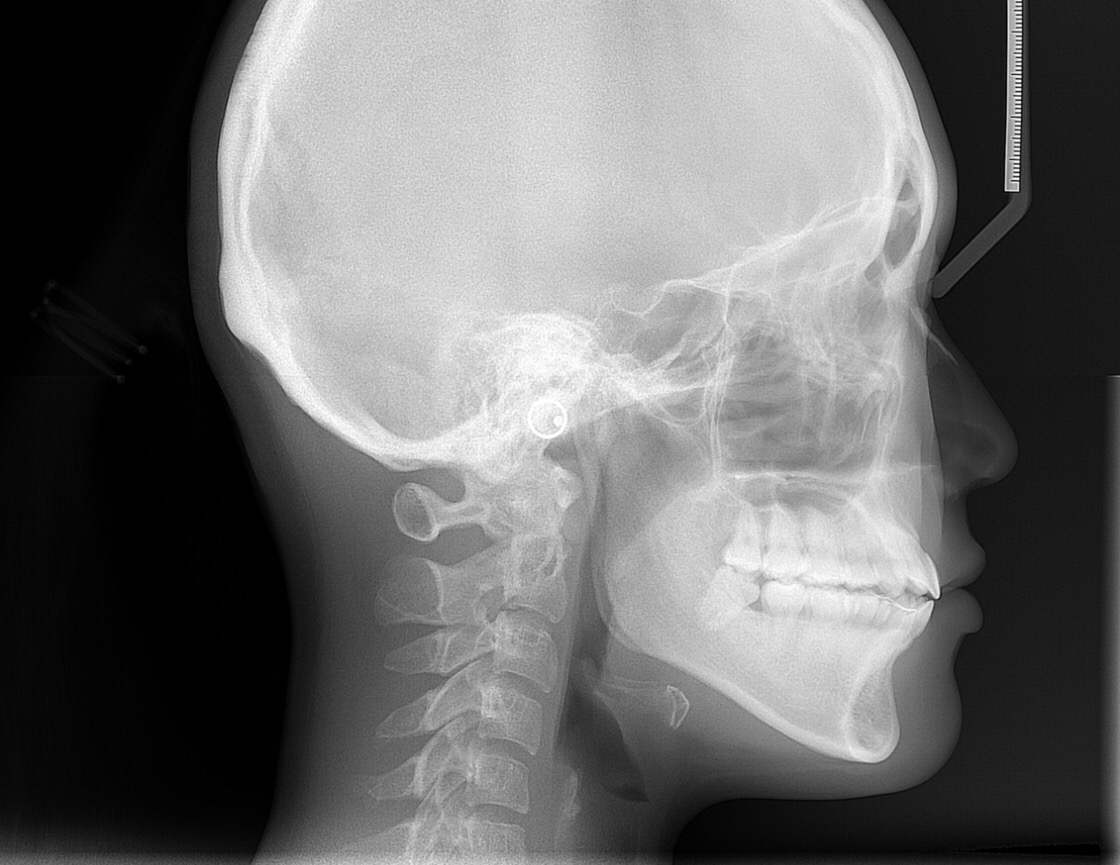
Part of planning for your retainer will be keeping records on hand like models and cephalometric x-rays. The extra angles of interpretation allow you to take various orofacial anatomical structures into consideration: not just the alignment of the teeth. Not to mention that digital ceph films can easily (and securely) be stored in the cloud by off-site providers like CephX for you to conveniently access them anytime in the future. When and if anything needs to be analyzed or re-analyzed months to years down the road, the data is available at your fingertips.
Follow Up Appointments: Make Them Worthwhile
Once an adult or teenager gets out of braces, most orthodontists never see or hear from them again…unless there’s a problem. The best way to avoid common problems — like lost or broken retainers, and tooth relapse — is to intermittently assess their bite.
Like a jeweler who inspects a wedding ring or diamond jewelry once a year to ensure that the prongs are holding everything in place, an orthodontic patient can benefit from having his or her bite reassessed on an annual basis from their orthodontist.
The intermittent appointments allow you to monitor retainer use, oral hygiene, maintenance of their prosthesis, and if any adjustments need to be made. As with other type of dental appliances, an orthodontic retainer can gradually wear out or break. Communicate with your patient that this is normal, and they need to have a new retainer made 5-10 years down the road. You might even want to consider offering the retainer for free as a “courtesy” to people who make their annual follow-up appointments and have been wearing their previous retainer on a routine basis.
Retention is for Life
It can’t be emphasized too much: an orthodontic retainer needs to be worn regularly for life. Even if it’s 20 years down the road, this must be stressed to your patients. Unfortunately, many orthodontic offices do not push this concept enough. As such, many adults come back for re-treatments due to lack of retention strategies following treatment as a teenager or busy college student.
For individuals that have — or still are battling — oral health conditions such as periodontitis or TMJ disorder, maintaining proper tooth placement is part of a comprehensive approach to their overall dental care. Be sure to get their family dentist or specialist on board by sending a letter back to their practice once your treatment has been completed. If you haven’t heard from the patient in a while, consider asking his or her dental provider to refer them back for a follow-up appointment.
Implementing Digitally Advanced Strategies to Enhance Care
In the days of digital patient information and images, it’s important to know that your patients’ data can be stored safely and securely…especially when you don’t see them for months at a time. At CephX, our cloud based record keeping systems are secured and accessible from any device, anywhere in the world. Now you can securely back up your patients’ old x-rays and other records without them taking up extra space in your office. Contact us today to learn more about our digital AlgoCeph analysis and more.