What is Cephalometric Analysis?
Cephalometric analysis is commonly used by dentists and orthodontist to study skeletal relationships in the craniofacial complex. However, cephalometric analysis also has many other uses. They can be uses to predict future changes, study the success of ongoing treatment plans, evaluate a patient’s dentofacial proportions and help doctors recognize abnormalities.
For these reasons, cephalometric analysis is paramount when developing and evaluating proper treatment plans for patients. Yet understanding how to do a cephalometric analysis properly is often the most difficult obstacle for many doctors.
Before learning how to do a cephalometric analysis, it is important to understand the basics of the procedure. A cephalometric analysis consists of two parts: the initial x-ray examination and the post-examination reading. The reading uses angular, linear, coordinate, and arcial relationships to reveal critical information about the maxillary position, mandibular position, facial proportions/vertical relationships, and incisor positions (both maxillary and mandibular) of a patient.
By using a comparative set of angles and distances, measurements can be related to one another and to normative values to determine variations in a patient’s facial structure. So, here’s how to do a cephalometric analysis of your own.
Part 1: The Cephalostat
The first step is to examine patients in a cephalostat according to the worldwide standard measurements for a cephalometric analysis. Following the standards ensure that all radiographs have the same diagnostics. Position the patient’s skull at a 90-degree angle to the X-ray beam, at a five foot distance from the tube, and place the film 15 inches from the patient’s head.
Although many doctors place emphasis on the post-examination analysis, it’s important to remember that if the X-rays are not accurate, it will be impossible to generate a correct analysis!
Part 2: Post-examination analysis
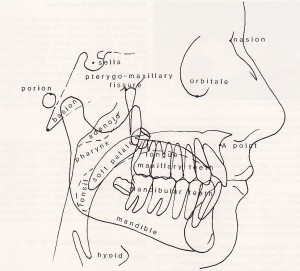
The analysis of the radiographs is one of the significant and difficult parts of the cephalometric analysis. After taking an X-ray of the skull, it is necessary to trace the film at multiple angles using either the computer’s drawing tool or a small diameter (0.5mm) pencil or pen. Tracings must be at a 1:1 ratio to the radiograph.
When tracing, ensure all lights are turned off and areas around the radiograph are darkened so that the reading is clear. Marking anatomical structures clearly and accurately is of paramount importance, because the angles and reference lines depend on their accuracy.
Outline the following areas carefully:
- The soft tissue profile of the patient’s face (from forehead to chin)
- The sella turcica
- The frontal bone and nasal bone
- The orbital floor
- The external auditory meatus
- The maxilla (both the upper first molar and the upper central incisor)
- The mandible, mandibular symphysis (the lower first molar and lower central incisor).
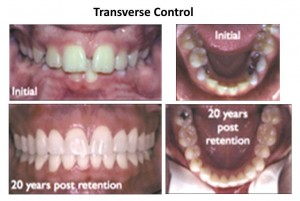
After outlining all the designated areas, designate the lines and planes and compare these to normal values to determine the patient’s deviation from the standard. Additionally, doing multiple cephalometric analysis with one patient over time allows you to understand the change and growth in a patient as well as diagnose how a patient is responding to treatment.
This can also reveal vital responses before, during, and after orthodontic treatment as well as be used to observe pathologic changes. It is typically recommended to perform two to three cephalometric analyses over 6-12 month intervals when assessing a patient’s readings over time.
Cephalometric Measurements
Cephalometrics aims to better understand how structures of the skull work by comparing a patient’s specific measurements with general averages. Measurements are an extremely important part of the cephalometric process, because an individual patient’s measurements are compared to population norms to spot deviations and assess where dental and orthodontic issues are occurring.
During a cephalometric x-ray, doctors must adhere to protocols to ensure that a patient’s results can be accurately compared with the general mean. While there is one standard for measurement during the x-ray, there are many different points of measurement for the radiograph during the post x-ray analysis.
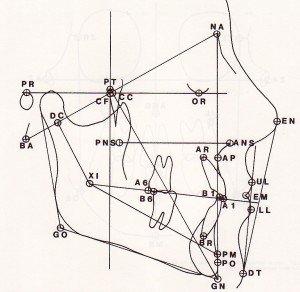
The points of measurement have been popularized throughout time by different cephalometric experts, and some sets of analyses are now more commonly used than others. Steiner’s, Downs, Tweeds, and Ricketts analyses are among some of the most popular. Each of these use different sets of measurements following specific landmarks in the bony and soft tissues of the skull to create angles of comparison.
In cephalometrics, the landmarks, or points of measurement, often demonstrate the relationship of the maxillary teeth and mandibular teeth, the jaws to the teeth and the jaws to one another, and the jaws to the cranial base. By drawing a complex series of angle and plane values, doctors are able to create values to compare for each measurement series.
What do cephalometric measurements do?
- Point out the location of imbalances or irregularities
- Demonstrate whether malocclusions are due to skeletal or alveolar deviations
- Show whether dysplastic development or dento-alveolar compensation causes skeletal discrepancy in patients
- Identify possible areas of asymmetry
- Show relationship between facial structures
- Help doctors gain understanding causes of facial issues (if any)
Correctly identifying cephalometric measurements can make or break an analysis, which is why many medical professionals have turned to electronic help to ensure that measurements are drawn accurately. Additionally, by locating measurements digitally, doctors can easily compare a patient’s ceph to normative values across gender, sex, and other demographic averages. Digitally tracing cephalometric radiographs ensures measurements have no mistakes and is a great tool for medical professionals today.
Cephalometric Analysis and Remote Tracing
Tracing a cephalometric radiograph has traditionally been one of the most tedious and time consuming parts of any cephalometric exam. While the initial x-ray can be completed within minutes, the post X-ray analysis can take much longer. A cephalometric tracing can be produced either by digital means or by the more traditional hand-drawing method, and it results in a superimposed drawing over the original cephalometric radiograph. Cephalometric tracings outline the particular measurements, landmarks, and angles that medical professionals need to use a ceph in treatment.
As many know, hand tracing is not only time consuming but runs an enormous risk of inaccuracies due to inevitable human errors. Many doctors have now turned to electronic tracing as a way to save time and reduce errors.
Now, you don’t have to worry about tracing or processing cephs in-house – let CephX do the work for you. CephX offers a complete solution to trace, analyze, store, and track your patients’ cephs.
With Remote Tracing Service (RTS), CephX ensures you can get the analysis you need without the hassle. Trust the experts to get your cephs traced accurately, quickly, and error free. How does it work?
- Simply upload a new ceph to your account.
- Within 2 business days, you will be receive your analysis.
- You will be able to view, edit and print all standard cephalometric analysis.
What are the benefits of using RTS?
Instead of wasting precious time trying to analyze, upload, and track patients’ cephs yourself, send it to experts who are here to make your job easier. All of your cephs will be stored securely in the cloud, which means anyone with account access can view, edit, or print the analysis. No more chasing information around the office – simply provide CephX cloud account information, and anyone can access the cephs. You don’t have to worry about losing physical copies of ceph analysis, because a copy will be stored securely on the cloud. Furthermore, with CephX, you can request custom analysis beyond the 60 standard cephalometric analysis offered.
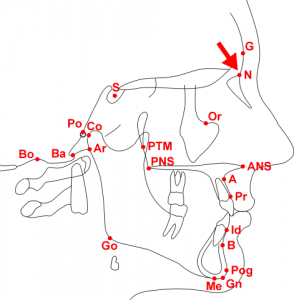
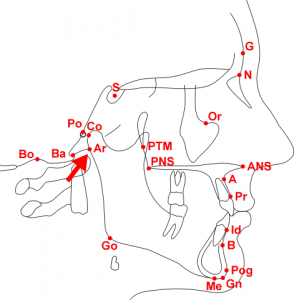
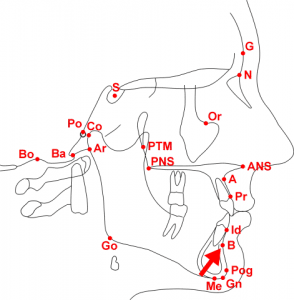
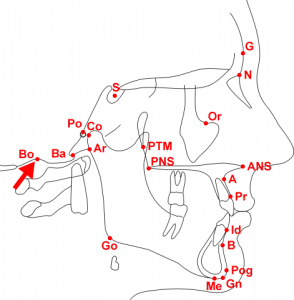
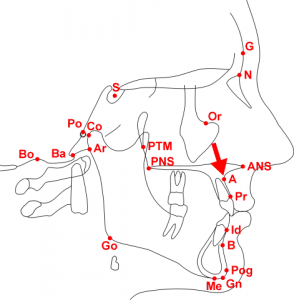
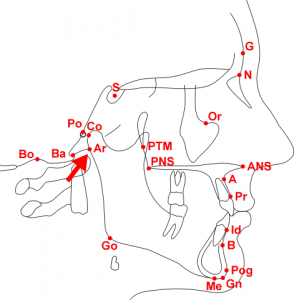
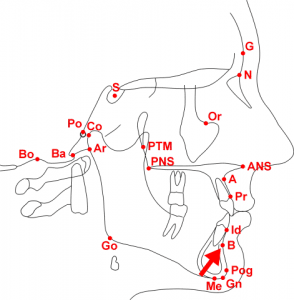
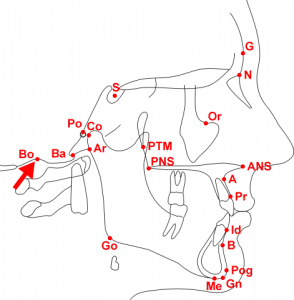
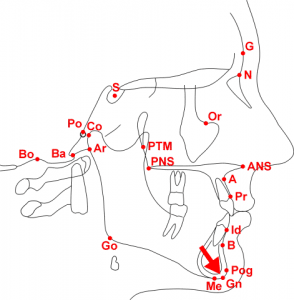
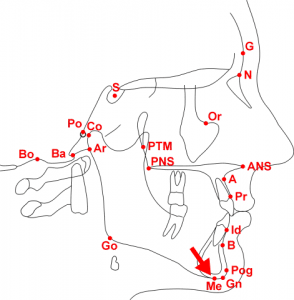
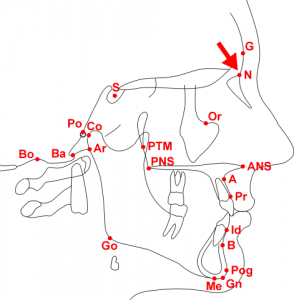
Cephalometric Analysis landmarks
Readily recognizable points on a cephalometric radiograph or tracing, representing certain hard or soft tissue anatomical structures (anatomical landmarks) or intersections of lines (constructed landmarks). Landmarks are used as reference points for the construction of various cephalometric lines or planes and for subsequent numerical determination of cephalometric analysis measurements.
In the definitions of the specific landmarks the following convention is used: “midsagittal” identifies landmarks lying on the midsagittal plane, “unilateral” identifies landmarks corresponding to unilateral structures and “bilateral” applies to landmarks corresponding to bilateral structures.
SUBTERMS:
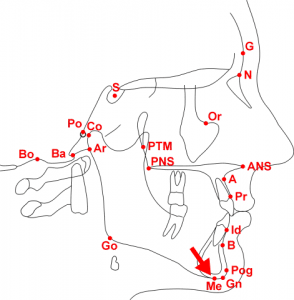
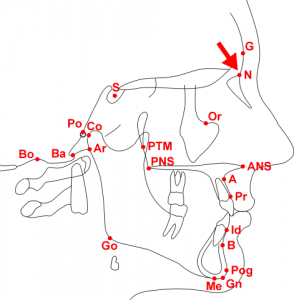
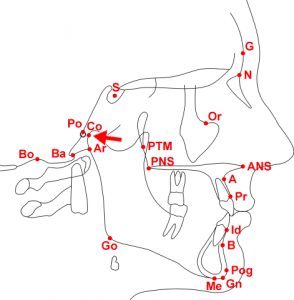
A-point (Point A, Subspinale, ss)
Anterior nasal spine (ANS)
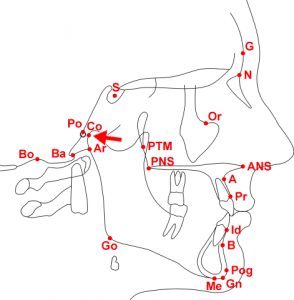
Articulare (Ar)
B-point (Point B, Supramentale, sm)
Basion (Ba)
Bolton (Bo)
Condylion (Co)
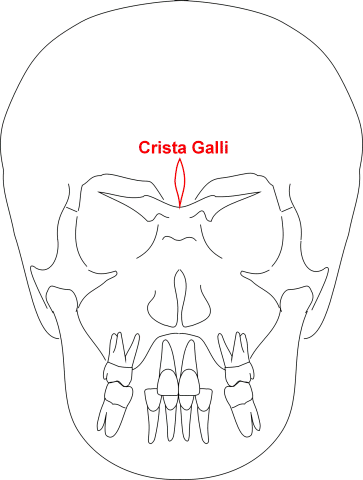
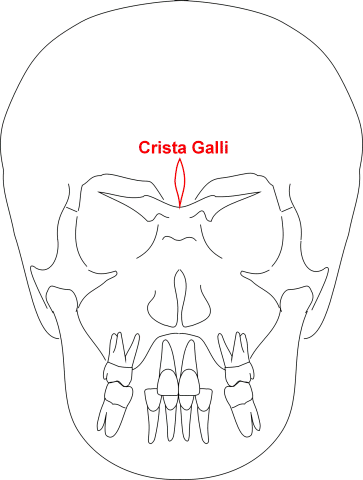
Crista galli
Dacryon
Glabella (G)
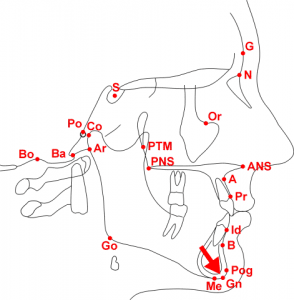
Gnathion (Gn)
Gonion (Go)
Incision inferius (Ii)
Incision superius (Is)
Infradentale (Id, Inferior prosthion)
L-point
Menton (Me)
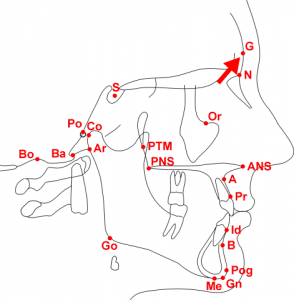
Nasion (N, Na)
Opisthion (Op)
Orbitale (Or)
Pogonion (Pog, P, Pg)
Porion (Po)
Posterior nasal spine (PNS)
Prosthion (Pr, Superior prosthion, Supradentale)
Pterygomaxillary fissure (PTM, Pterygomaxillare)
R-point (Registration point)
Sella (S)
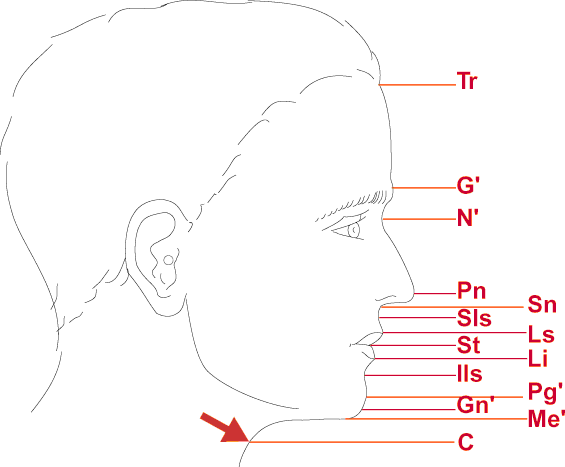
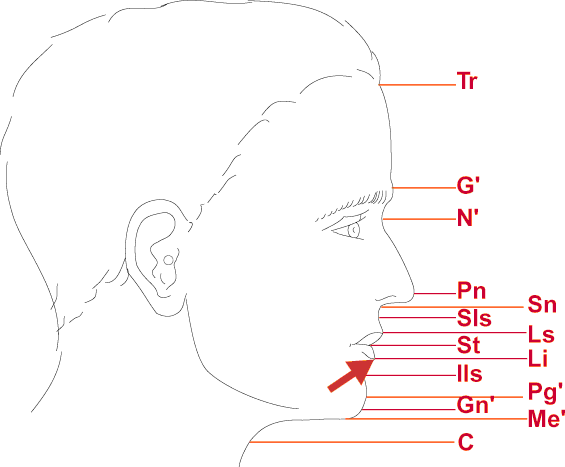
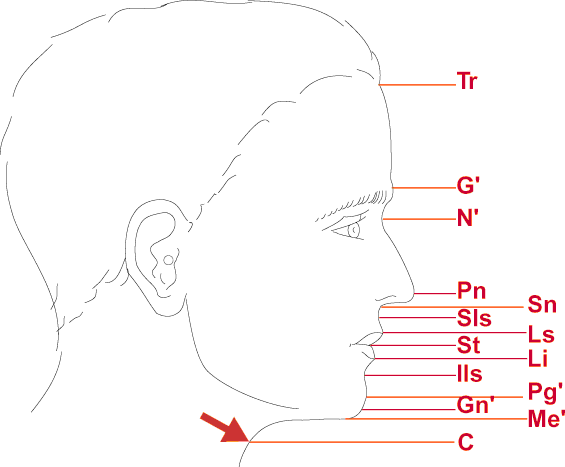
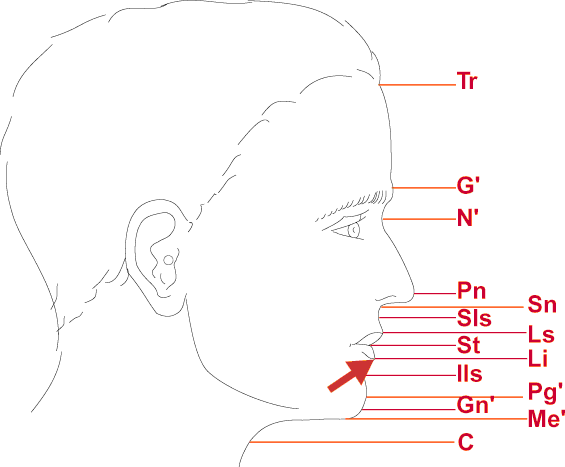
Cervical point (C)
Inferior labial sulcus (Ils)
Labrale inferior (Li)
Labrale superior (Ls)
Pronasale (Pn)
Soft tissue glabella (G’)
Soft tissue menton (Me’)
Soft tissue nasion (N’, Na’)
Soft tissue pogonion (Pg’, Pog’)
Stomion (St)
Stomion inferius (Sti)
Stomion superius (Sts)
Subnasale (Sn)
Superior labial sulcus (Sls)
Trichion (Tr)
Soft tissue gnathion (Gn’)
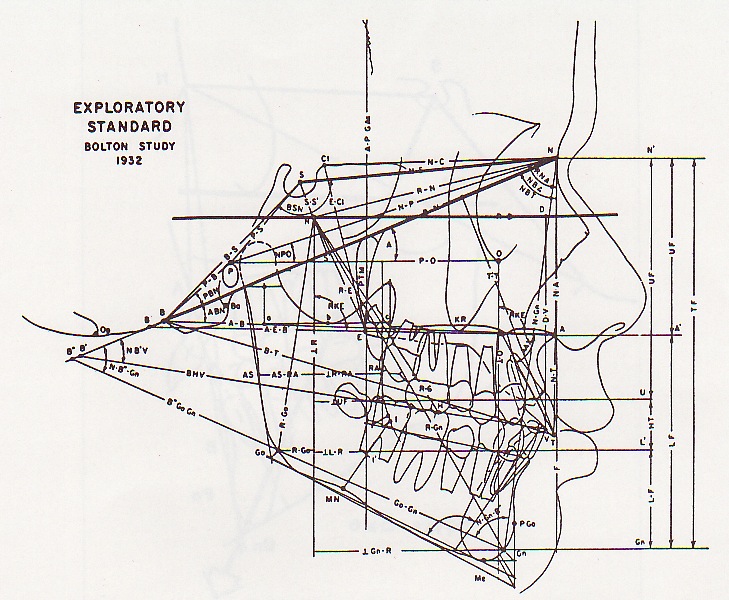
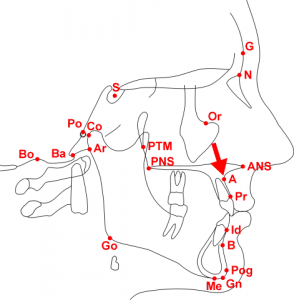
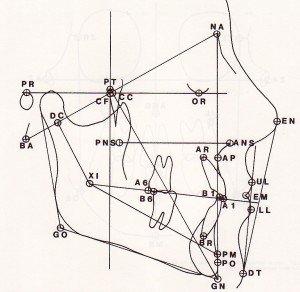
Ricketts Anatomical Tracing
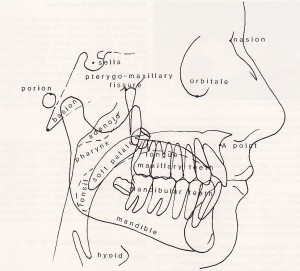
Ricketts Points and Planes
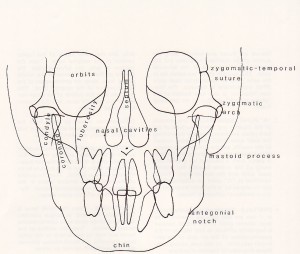
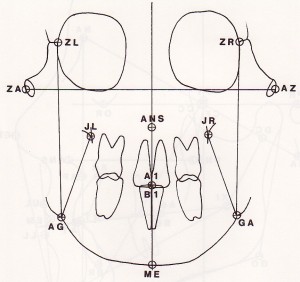
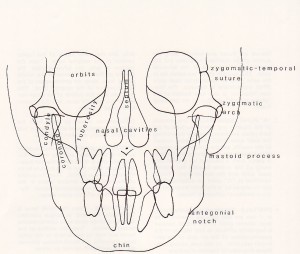
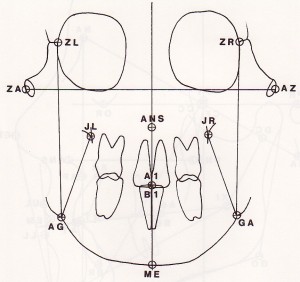
Ricketts Frontal Anatomy
A-POINT (POINT A, SUBSPINALE, SS)
The deepest (most posterior) midline point on the curvature between the ANS and prosthion. Its vertical coordinate is unreliable and therefore this point is used mainly for anteroposterior measurements. The location of A-point may change somewhat with root movement of the maxillary incisor teeth. (midsagittal)
ANTERIOR NASAL SPINE (ANS)
The tip of the bony anterior nasal spine at the inferior margin of the piriform aperture, in the midsagittal plane. It corresponds to the anthropological point acanthion and often is used to define the anterior end of the palatal plane (nasal floor). (midsagittal)
Articulare (Ar)
A constructed point representing the intersection of three radiographic images: the inferior surface of the cranial base and the posterior outlines of the ascending rami or mandibular condyles. It was meant to substitute condylion when the latter is not readily discernible. Any movement of the mandible (i.e. opening or closing) will change the location of articulare. (bilateral)
B-point (Point B, Supramentale, sm)
The deepest (most posterior) midline point on the bony curvature of the anterior mandible, between infradentale and pogonion. (midsagittal)
Basion (Ba)
The most anterior inferior point on the margin of the foramen magnum, in the midsagittal plane. It can be located by following the image of the slope of the inferior border of the basilar part of the occipital bone to its posterior limit, superior to the dens of the axis. (midsagittal)
Bolton (Bo)
The highest points on the outlines of the retrocondylar fossae of the occipital bone, approximating the center of the foramen magnum. Named after C. B. Bolton. (bilateral)
CC Point (CC) Ricketts
(Cranial Center) Crossing of the facial axis with the BaN plane
Cervical point (C)
The innermost point between the submental area and the neck in the midsagittal plane. Located at the intersection of lines drawn tangent to the neck and submental areas. (midsagittal)
Condylion (Co)
The most superior posterior point on the head of the mandibular condyle. (bilateral)
Crista galli
A vertically elongated, diamond-shaped radiopacity, appearing between the orbital outlines on postero-anterior cephalometric radiographs. Its location is used to establish a midsagittal reference plane. (midsagittal)
Dacryon
The point of intersection of the frontomaxillary, lacrimomaxillary and frontolacrimal sutures. An anatomic reference point used to record interorbital distance. (bilateral) Orbital hypertelorism
The increased distance between the medial orbital walls, reflecting an increased distance between the orbits (greater than 2 standard deviations from the norm). The anatomic landmarks used commonly for the measure-ment of interorbital distance are the dacryon points (bilaterally). Hypertelorism is described on the basis of skeletal measurements, because the presence of epicanthal folds or strabismus (exotropia), or other soft-tissue variations such as increased distance between the medial canthi (telecanthus) clinically may give a false impression of hypertelorism. Orbital hypertelorism is common in a number of craniofacial malformations such as Crouzon syndrome and frontonasal dysplasia.
Compare with Telecanthus
DC Point (Ricketts)
Center of the neck of the condyle on the Basion Nasion line.
Glabella (G)
The most prominent point of the anterior contour of the frontal bone in the midsagittal plane. (midsagittal)
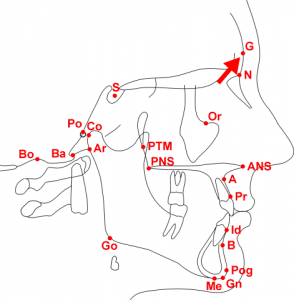
Gnathion (Gn)
The most anterior inferior point on the bony chin in the midsagittal plane. (midsagittal)
Gonion (Go)
The most posterior inferior point on the outline of the angle of the mandible. It may be determined by inspection or it can be constructed by bisecting the angle formed by the intersection of the mandibular plane and the ramal plane and by extending the bisector through the mandibular border. (bilateral)
Infradentale (Id) Inferior prosthion Pr
The most superior anterior point on the mandibular alveolar process, between the central incisors. (midsagittal)
Incision inferius (Ii) or B1 (Ricketts)
The incisal tip of the most labially placed mandibular incisor. (unilateral)
Incisian Inferius Root or BR (Ricketts)
Incision superius (Is) or A1 (Ricketts)
The incisal tip of the most labially placed maxillary central incisor. (unilateral)
Incision Superious Root or AR (Ricketts)
L-point
A point located in the anterior surface of the cortical plate, labial to the apices of the maxillary central incisors. Introduced by F. P. G. M. van der Linden, as a point representing the anterior border of the maxillary apical area. (midsagittal)
Labrale inferior (Li)
The point denoting the vermilion border of the lower lip, in the midsagittal plane. (midsagittal)
Labrale superior (Ls)
The point denoting the vermilion border of the upper lip, in the midsagittal plane. (midsagittal)
Menton (Me)
The most inferior point of the mandibular symphysis, in the midsagittal plane. (midsagittal)
Molar Upper First (Ricketts)
Point on the occlusal plane perpendicular to the distal surface of the crown of the upper first molar.
Molar Lower First (Ricketts)
Point on the occlusal plane perpendicular to the distal surface of the crown of the lower first molar.
Nasion (N, Na)
The intersection of the internasal and frontonasal sutures, in the midsagittal plane. (midsagittal)
Opisthion (Op)
The most posterior inferior point on the margin of the foramen magnum, in the midsagittal plane. (midsagittal)
Orbitale (Or)
The lowest point on the inferior orbital margin. (bilateral)
Pogonion (Pog, P, Pg)
The most anterior point on the contour of the bony chin, in the midsagittal plane. Pogonion can be located by drawing a perpendicular to mandibular plane, tangent to the chin. (midsagittal)
Porion (Po)
The most superior point of the outline of the external auditory meatus (“anatomic porion”). When the anatomic porion cannot be located reliably, the superior-most point of the image of the ear rods (“machine porion”) sometimes is used instead. (bilateral)
Posterior nasal spine (PNS)
The most posterior point on the bony hard palate in the midsagittal plane; the meeting point between the inferior and the superior surfaces of the bony hard palate (nasal floor) at its posterior aspect. It can be located by extending the anterior wall of the pterygopalatine fossa inferiorly, until it intersects the floor of the nose. (midsagittal)
Pronasale (Pn)
The most prominent point of the tip of the nose, in the midsagittal plane. (midsagittal)
Prosthion (Pr, Superior prosthion, Supradentale)
The most inferior anterior point on the maxillary alveolar process, between the central incisors. (midsagittal)
Protruberance Menti (Pm) or Supra pogonion (Ricketts)
A point where the curvature of the anterior border of the symphysis changes from concave to convex,
Pterygoid Point (Pt) Ricketts
Lower lip of foramen rotundum (Represents the position of the sphenoid bone) posterior superior tangent of the pterygomaxillary fissure
Pterygoid Root (Pr) Ricketts
Most posterior point on the outlines of the pterygopalatine fossa
Pterygomaxillary fissure (PTM, Pterygomaxillare)
A bilateral, inverted teardrop-shaped radiolucency, whose anterior border represents the posterior surfaces of the tuberosities of the maxilla. The landmark is taken at the most inferior point of the fissure, where the anterior and the posterior outline of the inverted teardrop merge with each other. (bilateral)
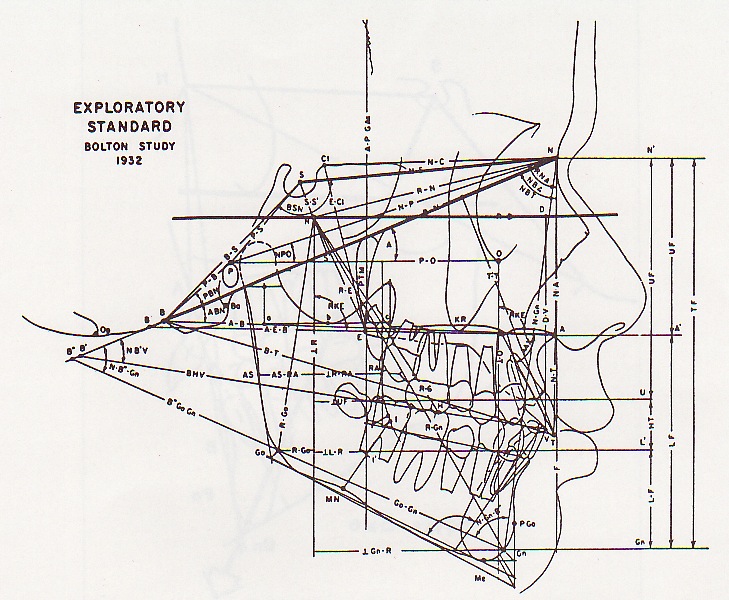
R-point (Registration point)
A cephalometric reference point for registration of superimposed tracings, introduced by B. H. Broadbent, Sr. , in his original presentation of the cephalometric technique. It is the midpoint on a perpendicular drawn from sella to the Bolton-nasion line. (midsagittal)
Sella (S)
The geometric center of the pituitary fossa (sella turcica), determined by inspectionóa constructed point in the midsagittal plane. (midsagittal)
Soft tissue glabella (Gí)
The most prominent point of the soft tissue drape of the forehead, in the midsagittal plane. (midsagittal)
Soft tissue menton (Meí)
The most inferior point of the soft tissue chin, in the midsagittal plane. (midsagittal)
Soft tissue nasion (Ní, Naí)
The deepest point of the concavity between the forehead and the soft tissue contour of the nose in the midsagittal plane. (midsagittal)
Soft tissue pogonion (Pgí, Pogí)
The most prominent point on the soft tissue contour of the chin, in the midsagittal plane. (midsagittal)
Stomion (St)
The most anterior point of contact between the upper and lower lip in the midsagittal plane. When the lips are apart at rest, a superior and an inferior stomion point can be distinguished. (midsagittal)
Stomion inferius (Sti)
The highest midline point of the lower lip. (midsagittal) if lips are apart
Stomion superius (Sts)
The lowest midline point of the upper lip. (midsagittal) if lips are apart
Subnasale (Sn)
The point in the midsagittal plane where the base of the columella of the nose meets the upper lip. (midsagittal)
Superior labial sulcus (Sls) Soft Tissue Point A
The point of greatest concavity on the contour of the upper lip between subnasale and labrale superius, in the midsagittal plane. (midsagittal)
Soft Tissue B or Inferior labial sulcus (Ils)
The point of greatest concavity on the contour of the lower lip between labrale inferius and menton, in the midsagittal plane. (midsagittal)
Trichion (Tr)
An anthropometric landmark, defined as the demarcation point of the hairline in the midline of the forehead. (midsagittal)
Xi Point (Xi) approximate for Inferior alveolar foramen (Ricketts)
A constructed point located at the geographic center of the ramus as indicated below.
Why cephX does it better?
CephX allows you to effortlessly order Cephalometric analyses without having to trace your cases manually and without having to purchase expensive software or hardware.
We are an easy to use, cloud based system that will provide you with accurate Cephalometric analyses, convenient image storage and on-demand patient records.
If you want to save costs while improving your practice and get unlimited access to your patient record anytime – Contact us for more info!