Common Psychological Aspects of Orthodontic Treatment -The Child, Adolescent and Adult Patient

As we all know, orthodontics is a long-term partnership. Psychological factors influence the choice of an orthodontist. Aside from protracted full mouth rehabilitation, most general and specialty dental procedures are done “to” the patient in a brief time and “as needed” rather than “with” the patient over a span of years.
This is not to say that non-orthodontic dental patients do not establish long term relationships with their dentists. Orthodontic-patient relationships necessarily have certain “dental” commonalities with non-orthodontic-patient relationships, but the difference lies mostly in long term related objectives with a resulting set of unique patient-practitioner psychological mindsets.
Basic Orthodontic Patient Psychology
Although it probably seems obvious to the average layman, numerous scientific studies have been undertaken that do confirm poor facial esthetics is related to:
- Low self-esteem.
- Problematic social activities/interactions.
- Adverse occupational outcomes.
That being true, it is not at all hard to appreciate that the main reason for the majority of orthodontic patients and parents to seek orthodontic treatment regardless of age is found to be the attainment (or improvement) of an attractive dental-facial relationship.
Basic motivational factors are influenced by:
- Social Environment.
- Gender
- Economic status
- Behavioral traits
- Personal issues
Basic motivational factors are influenced by:
Unless severe, functional issues of malocclusion having possible deleterious dental consequences often go unnoticed by individuals or parents. Even when apprised of functional issues, many patients or parents may not typically consider them enough of a key motivating factor(s) for the time and expense of undergoing treatment.
The Adult Patient
In the not so distant past, orthodontic treatment for adults was somewhat of a rarity.
Some of the past psychological and societal barriers to adult treatment included:
- “Braces are only for kids and teenagers”
- Occupational considerations
- Affordability
- Considered a “vanity”
- Appearance of metal braces
In contrast, it is estimated today that 1 in 5 patients in a typical orthodontic practice are adults with some practices reporting an adult patient level nearing 50 percent.
The advent of lingual braces and “invisible” dental aligners along with changing societal norms have allowed adults to overcome some of the psychological and societal prohibitions of appearing in public as an adult with a “full metal jacket” of traditional “old school” braces.
The Adolescent Patient
Adolescent psychology has long been a subject of interest to orthodontists. Like parents, it comes as somewhat of a surprise to them to see a relatively happy “well-adjusted” child patient gradually morph into a “whatever” teenager.
Up until the past 20 or so years, a common general layman’s perception was that of teenagers fearing the prospect of hearing the dreaded parental phrase, “You need braces!”. Visions of metal mouth teenagers being teased by their peers was a daunting prospect to both patient and parent. And there was and still is some truth to those characterizations even with modern orthodontic innovations.
Thankfully, psychological and societal norms have changed and rather than being a social detriment, wearing braces as a teenager has become an accepted norm. In fact, it is known through numerous social psychology and health science studies that peer pressure, rather than being a psychological barrier because of teasing etc., has now become one of the most powerful incentives and motivational factors leading teenagers to seek orthodontic treatment. Wearing braces has gone from just a means for improving facial esthetics to a positive social incentive with the extra bonus of now being an “in” thing.
Technical improvements have also made orthodontic treatment more psychologically acceptable for adolescents with the innovation of teen version dental aligners, clear brackets and the elimination of metal bands. There is also a current trend to make wearing more visible braces a fashion or personal statement with the introduction of various colored rubber bands, different shaped colored brackets, etc.

The Child Patient
Typically, child patients take their motivation for orthodontic treatment from their parents although that is not to say that some children do express concerns about the “crookedness” of their teeth. In the clear majority of cases, the mother is the parent that takes the lead in seeking consultation and treatment.
As with teenagers, the social stigma of the past regarding the wearing of braces among younger children has greatly decreased. One significant difference with the child patient is that peer pressure although a factor, does not seem to be a prime motivating social factor to the same degree as it is in adolescent patients.
The availability of colorful rubber bands, different shaped brackets and themed accessories (Spiderman, Hello Kitty) such as retainer boxes, toothbrushes, etc., can make the orthodontic experience less intimidating.
Orthodontist Concerns
Obviously for the orthodontist, the treatment for adults, adolescents and children entails the same end goal; proper establishment of functional orthodontic aspects as well as dental-facial esthetics. A basic understanding and use of adjunctive psychological approaches can be brought into play by the orthodontist to make these goals easier for the patient and more productive for the practitioner especially in the case of reticent patients and/or their parents.
Internal vs External Motivators
External
- Adult – perceived improved occupational opportunities, improved interpersonal relationships
- Adolescent – peer pressure, parental pressure, perceived improved interpersonal relationships
- Child – parental pressure.
Internal
- Adult – increased self-esteem, personal goal achievement, more attractive appearance
- Adolescent – social acceptance, self-actualization, more attractive appearance
- Child – parental approval, “better’ smile.
With each age group and patient appointment, the orthodontist will have unique opportunities to establish and maintain solid partnerships and increase patient rapport. These opportunities come through a basic understanding, continued study and application of patient-practitioner interactive psychology.
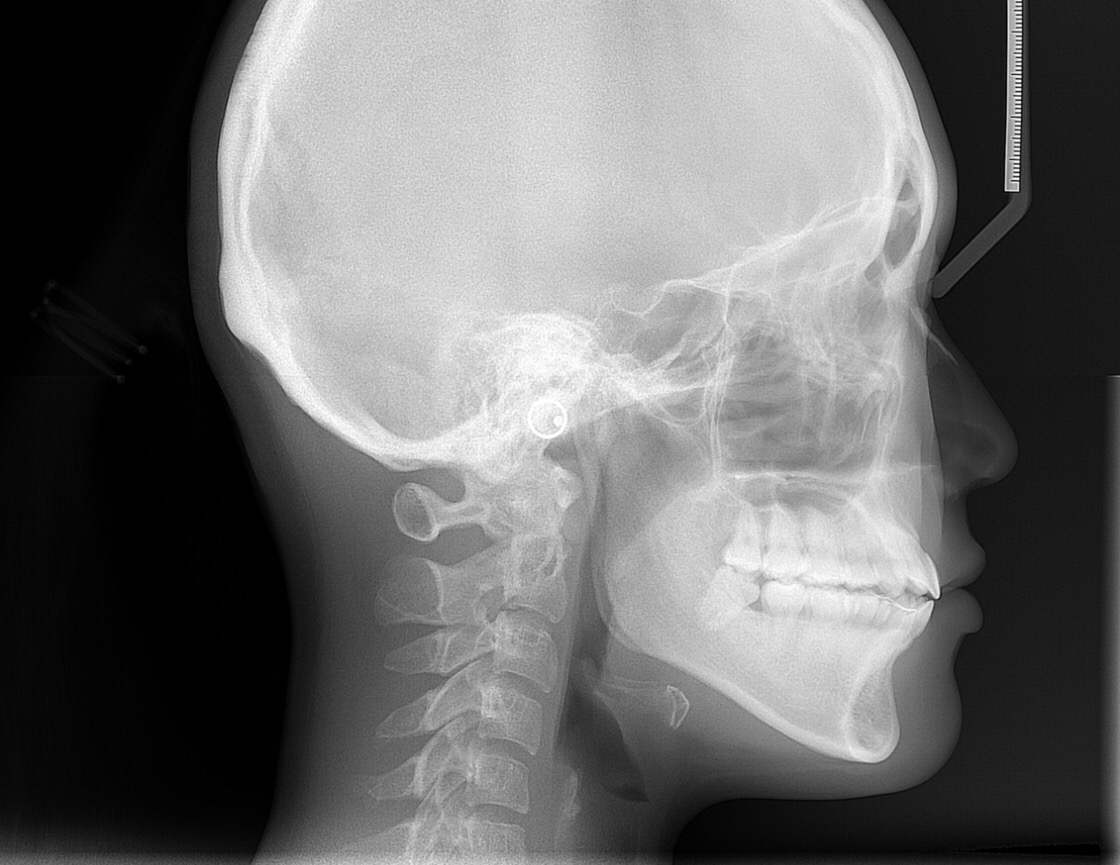
A busy practitioner needs every opportunity to increase the amount of time they can spend with their patients. They also need to keep abreast of modern technologies. Manual cephalometric analysis is very time consuming and can be stressful. Cephx online cephalometric analysis makes available 50 generic and custom analyses that can be managed from any device. Psychologically speaking from the viewpoint of that same busy orthodontist, besides freeing up some extra time for patient communication, using the services of a dedicated and trusted online cephalometric analysis company can help to take away some of the stress related to manual analysis. Cephx makes available their exclusive “Algoceph” algorithm and provides Cloud storage for seamless record retrieval. Visit our main website at: Cephx