Dr. Laura Nicolas
Dr. Alberto Teramoto
Department of Orthodontics. Universidad Latinoamericana Mexico City, Mexico.
Introduction
There is no doubt that resolving impacted teeth is very difficult with an inadequate treatment plan which lacks all necessary information. Moreover, it’s vital to know where impacted teeth are located and more importantly, what their relationship is to other teeth, roots and even the mandibular nerve.
After the third molars, maxillary canines have the highest frequency of impacted localization, with a prevalence ranging from 1% to 3% (1-4), and it is more frequent in female patients than male with a ratio of 2:1 (5). If surgical treatment is necessary, it requires a great deal of time and is a challenge to treat without the right information. This is why the accurate location of impacted maxillary canines is so crucial when deciding whether to treat orthodontically or with surgical intervention.
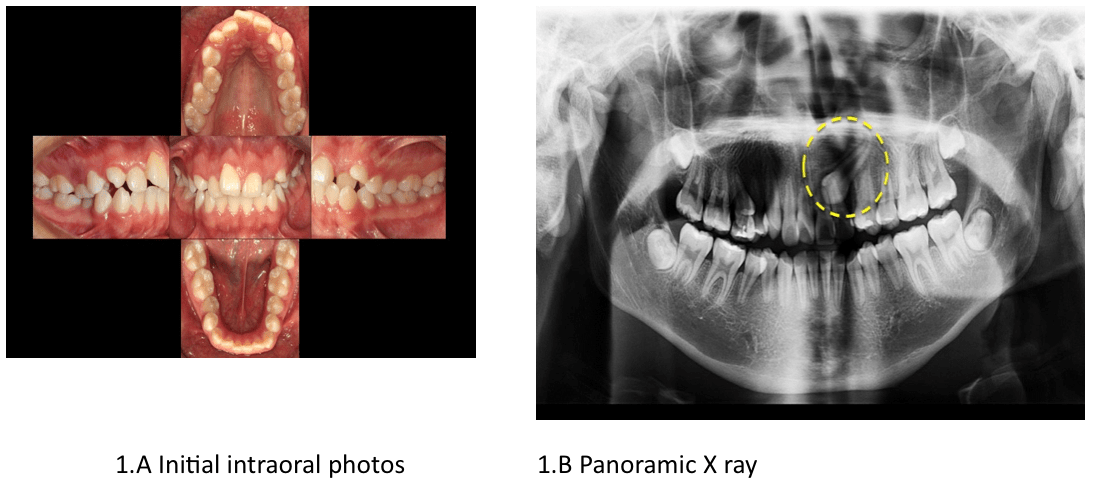
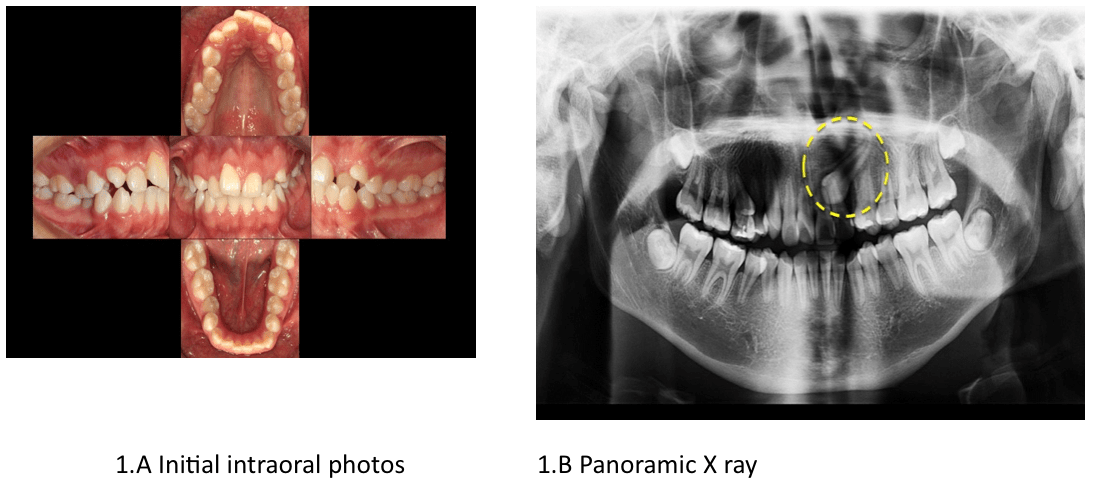
During our daily practice, the first radiographic image usually taken to support the clinical examination is the panoramic radiograph, and sometimes in order to have a better localization of impacted teeth, we can improve diagnosis by combining two or more bi-dimensional images such as: occlusal and periapical, which allow the localization of impacted canines, treatment planning, and evaluation of the treatment result.
Importance of CBCT
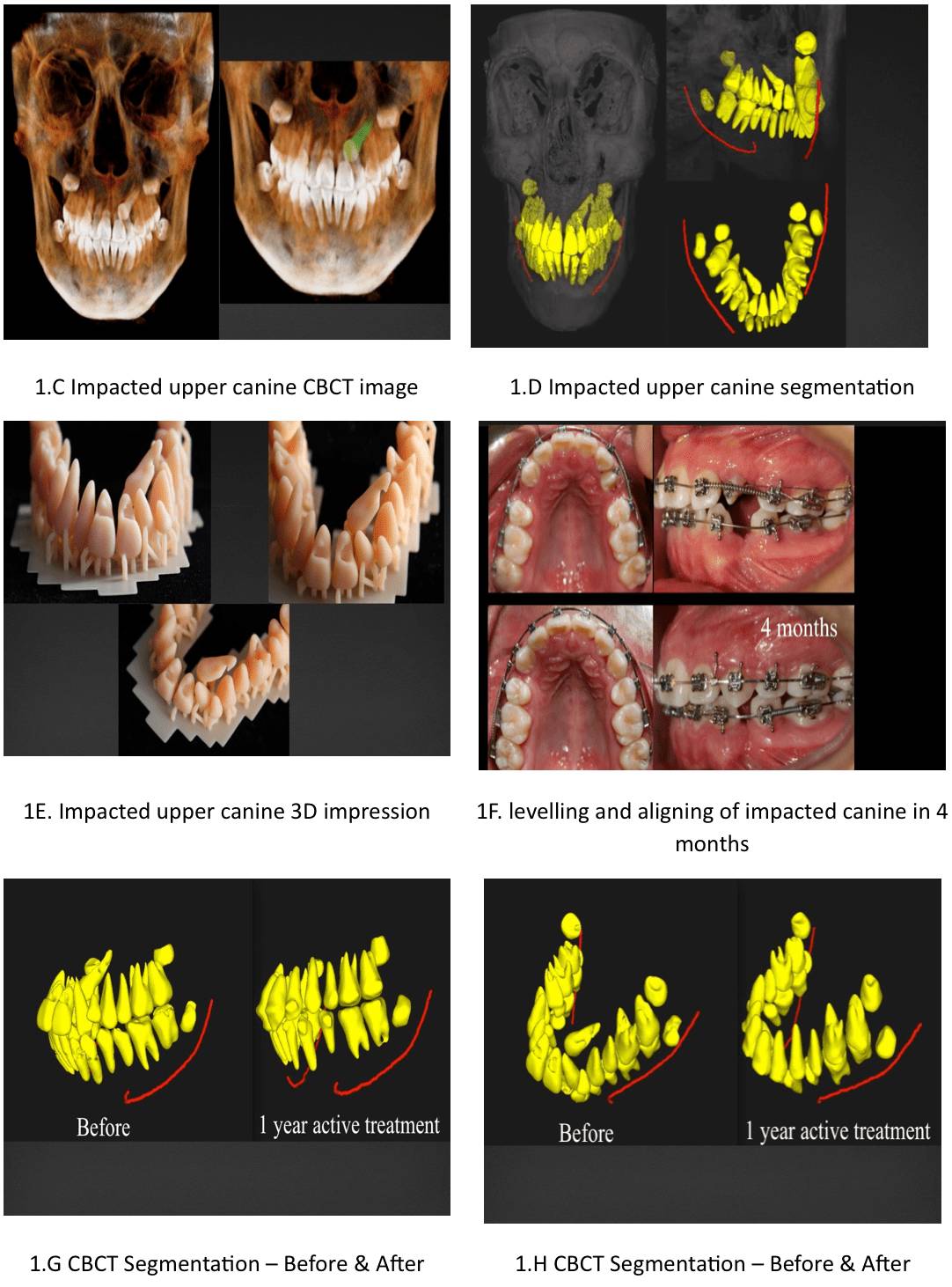
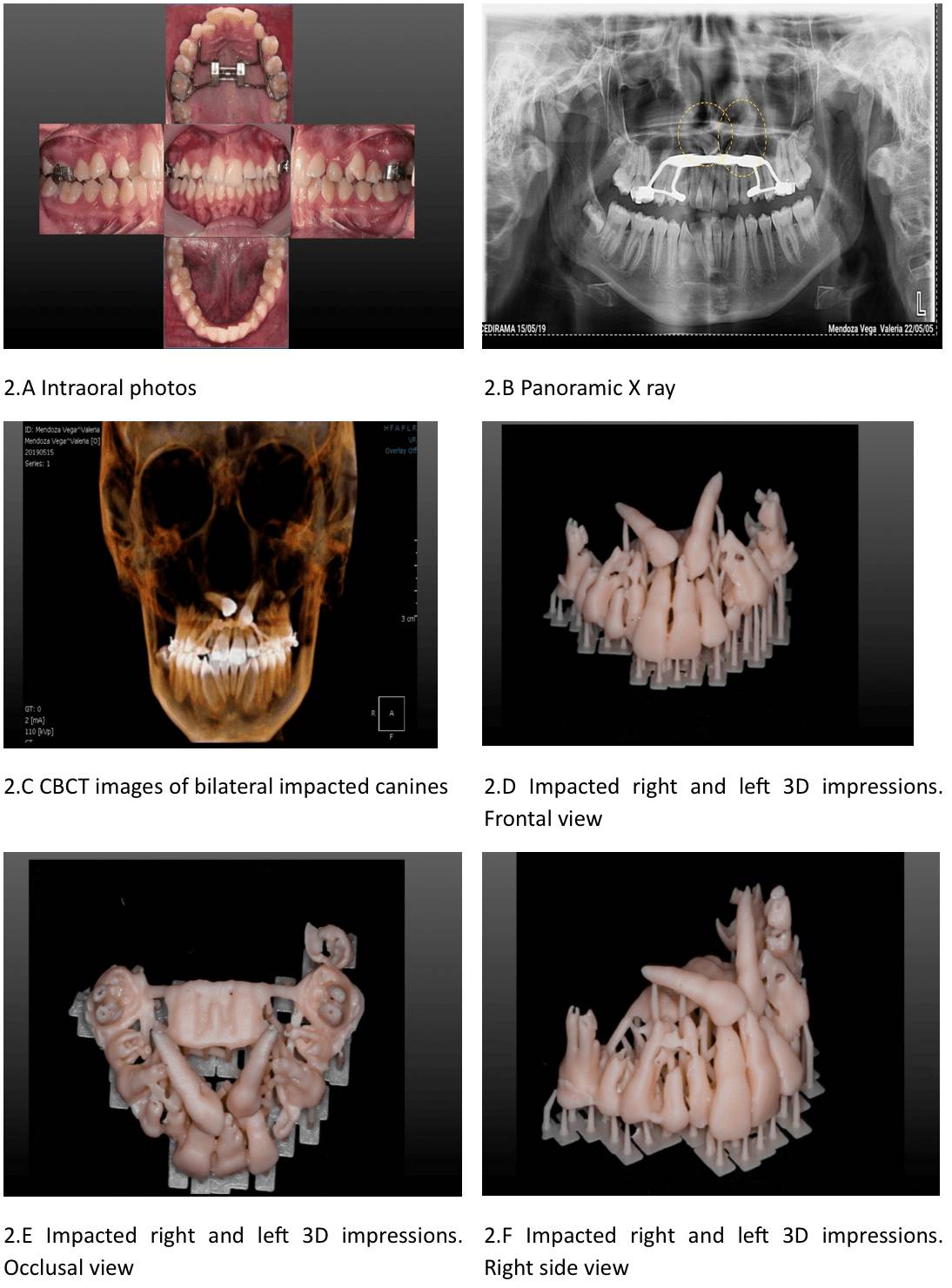
It is well known that the accuracy of these two-dimensional radiographic techniques is severely limited, increasing the risk of error. By adding a third dimension to the radiographic information, clinicians can improve diagnostic accuracy and treatment efficacy – using Cone Beam Computed Tomography (CBCT), clinicians can take advantage of 3D information provided by a low radiation dose, and at relatively low costs. CBCT provides information that is not revealed through traditional radiographic analysis, and is therefore recommended in cases of impacted teeth or craniofacial structural irregularities.
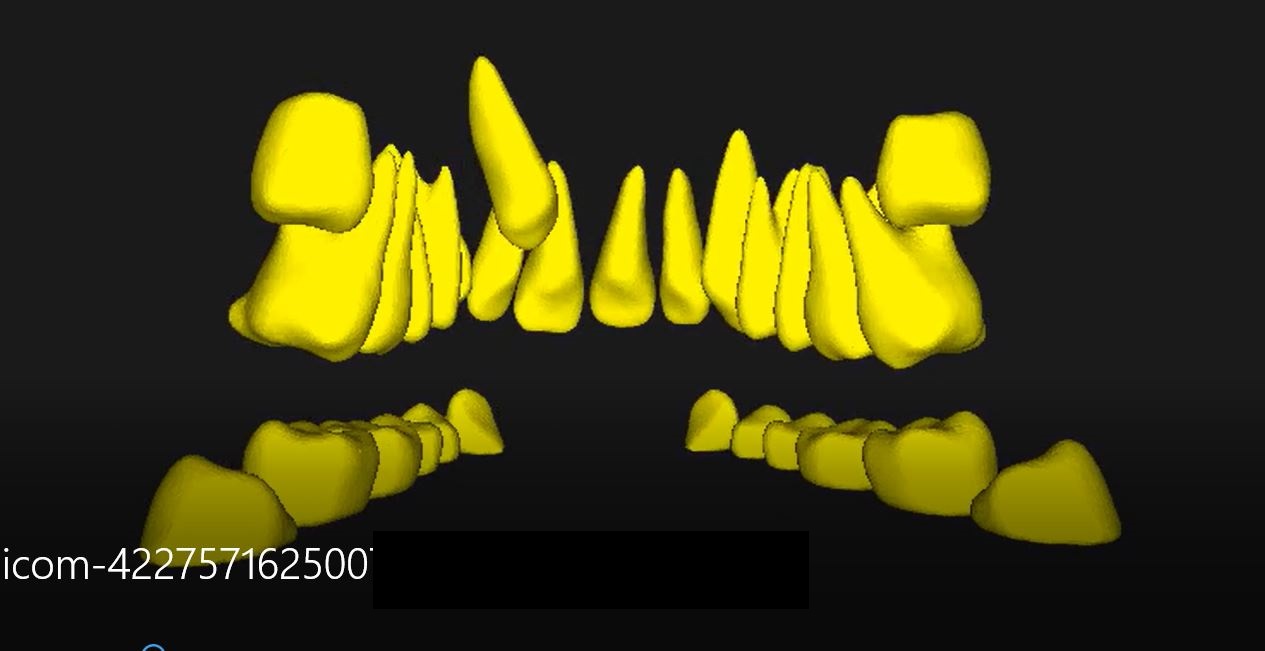
Although we have all these 3D images sometimes they are not enough, CBCT data offers much more than what we are able to use for imaging. DICOM data can also be used for segmentation, a process that separates structures of interest from the background and from each other, and for which a number of algorithms have been developed in image processing. Segmentation of an object is achieved either by identifying all pixels or voxels that belong to the object, or by locating those that form its boundary. Segmenting teeth is not an easy task. The following problems may arise when segmenting teeth from CBCT images:
1) DICOM data is acquired in upper-lower jaw in occlusion, so it is difficult to distinguish a tooth from its neighboring teeth along their occlusal surface due to the lack of gray-scale value changes.
2) It is also hard to separate a tooth from alveolar bone by similar densities.
3) Often, teeth possess similar shapes, making it difficult to identify different tooth types.
While there are many open source tools available for performing segmentation procedures, obtaining good quality segmentation takes time and requires a long learning curve.
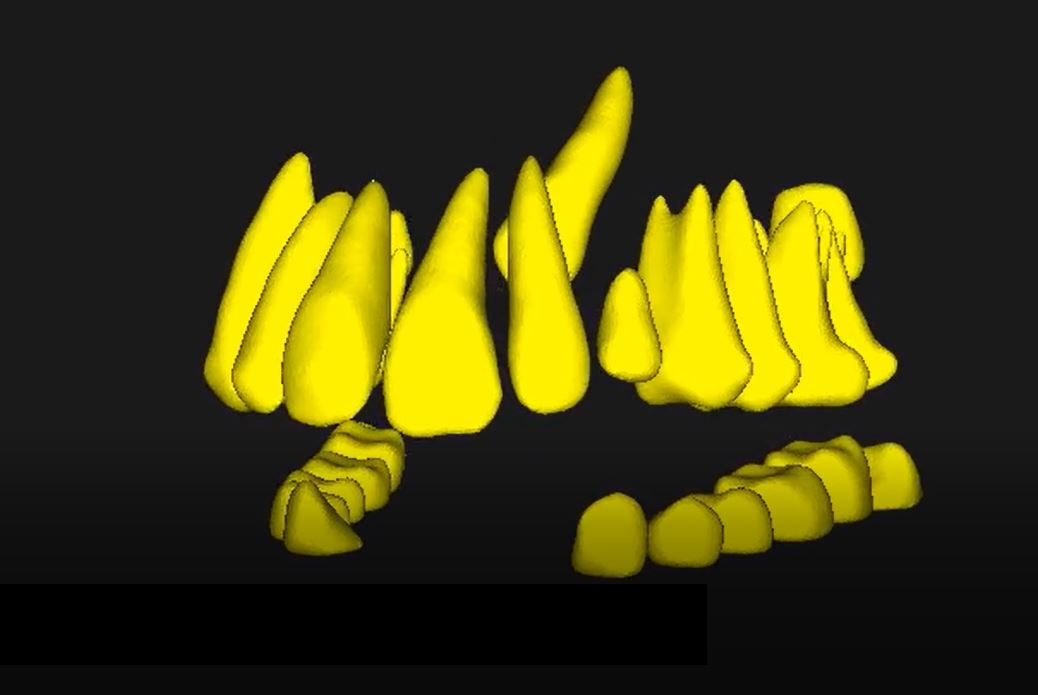
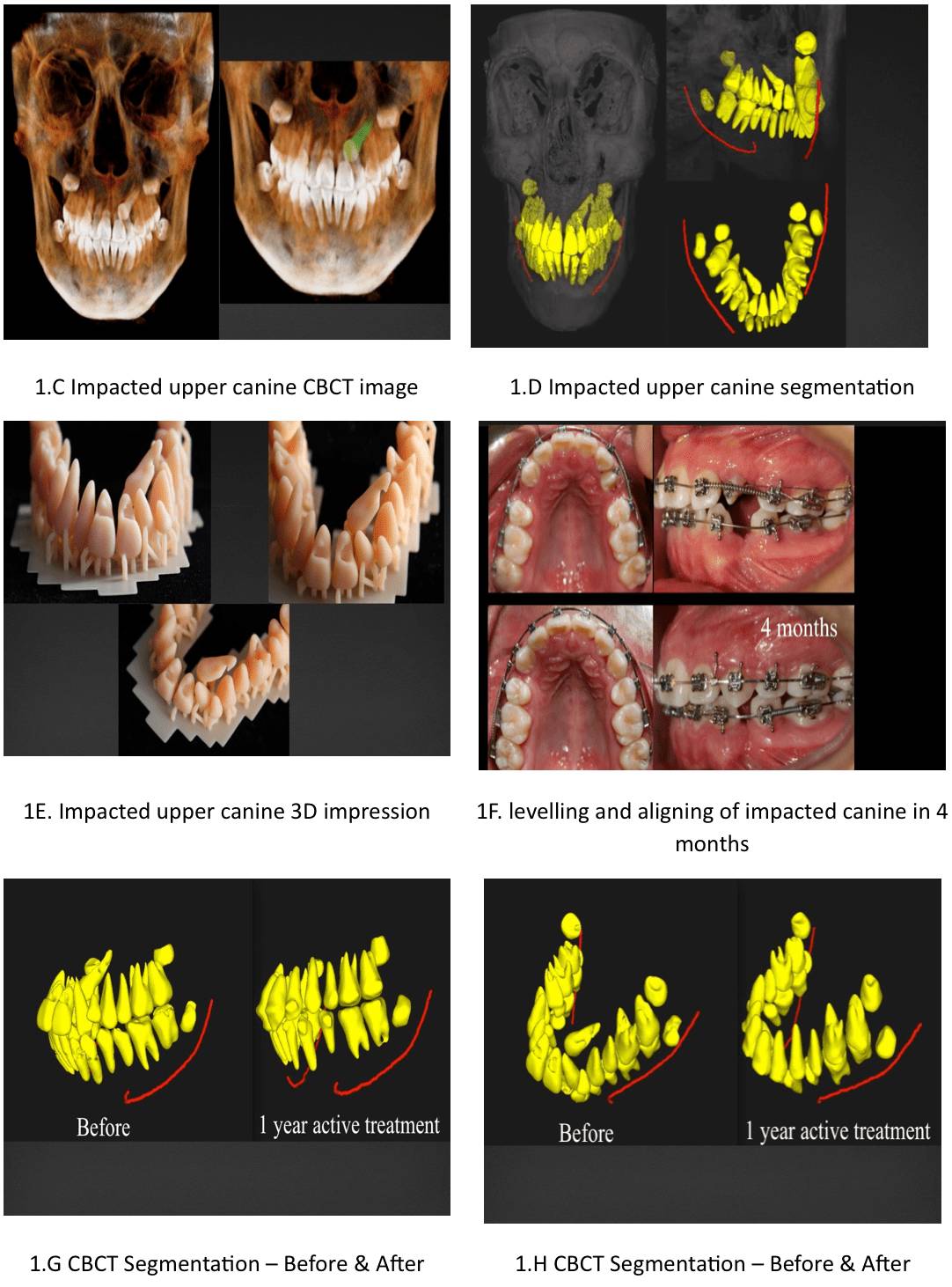
Using artificial intelligence technology, Orca Dental AI created a unique system in a 3D controllable STL format that includes not only teeth segmentation but also cephalometric and airway volume calculations, which make this process more comprehensive, easy to use and completely informative in disclosing all the impacted relationships.
To aid in an improved diagnostic approach and improve treatment outcomes, Data Imaging and Communication in Medicine (DICOM) files of the CBCT can also be converted into a 3D model using a 3D printer (Zenith D DENTIS Co. LTD). Therefore, this tool is very useful to visualize and be able to feel 3D conditions of teeth that are on the verge of falling out, since this process offers an extra diagnostic dimension. When analyzing this data, we can decide which is the best treatment plan, and for example decide if an orthodontic treatment to align an ectopic canine is better than a surgical procedure because ectopic canines are hard to align.
CASES
Case 1
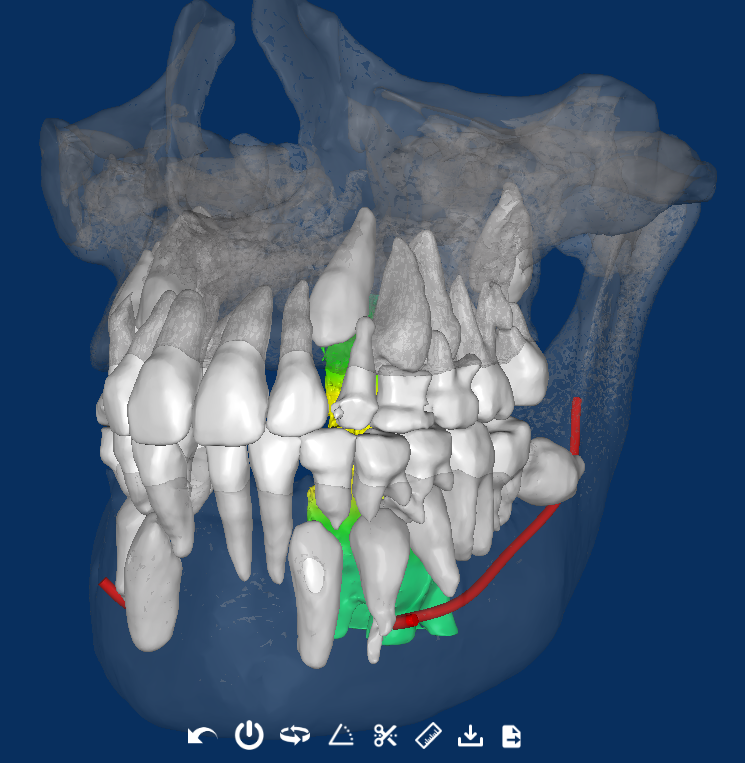
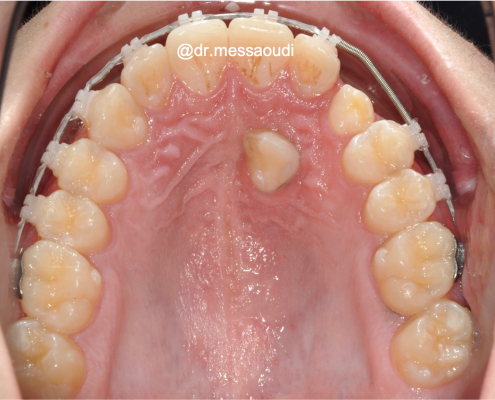
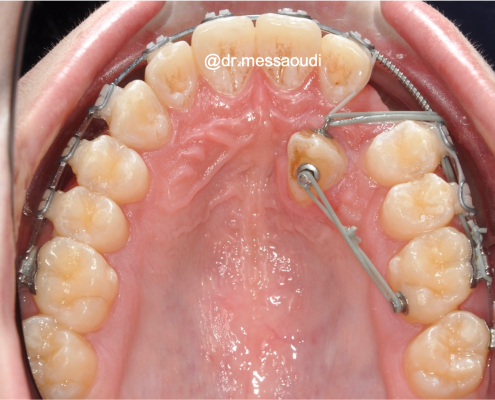
Since the root of the impacted canine is located close to the vestibular side, when the first premolar is extracted, the canine can easily be moved into its ideal position. (Fig.1 a-h)
Case 2
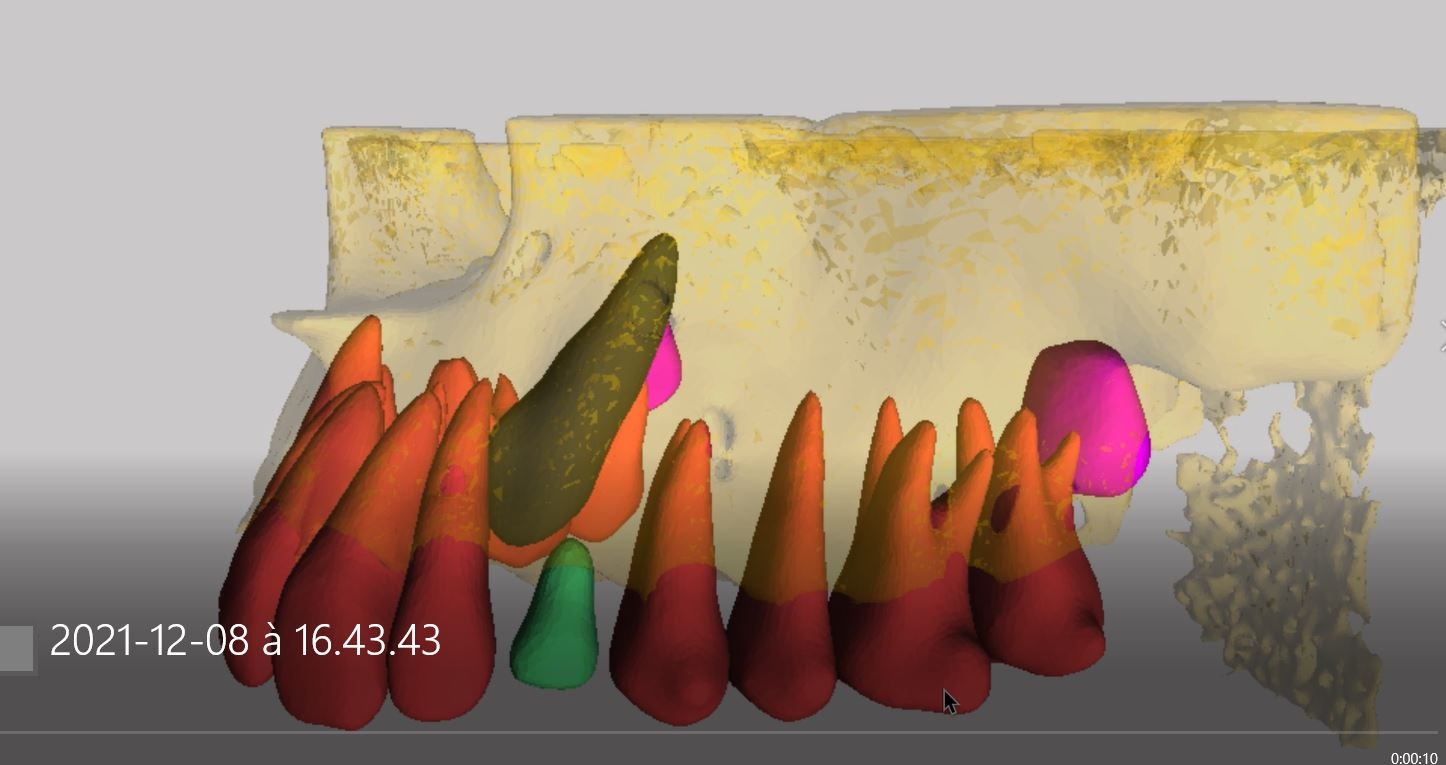
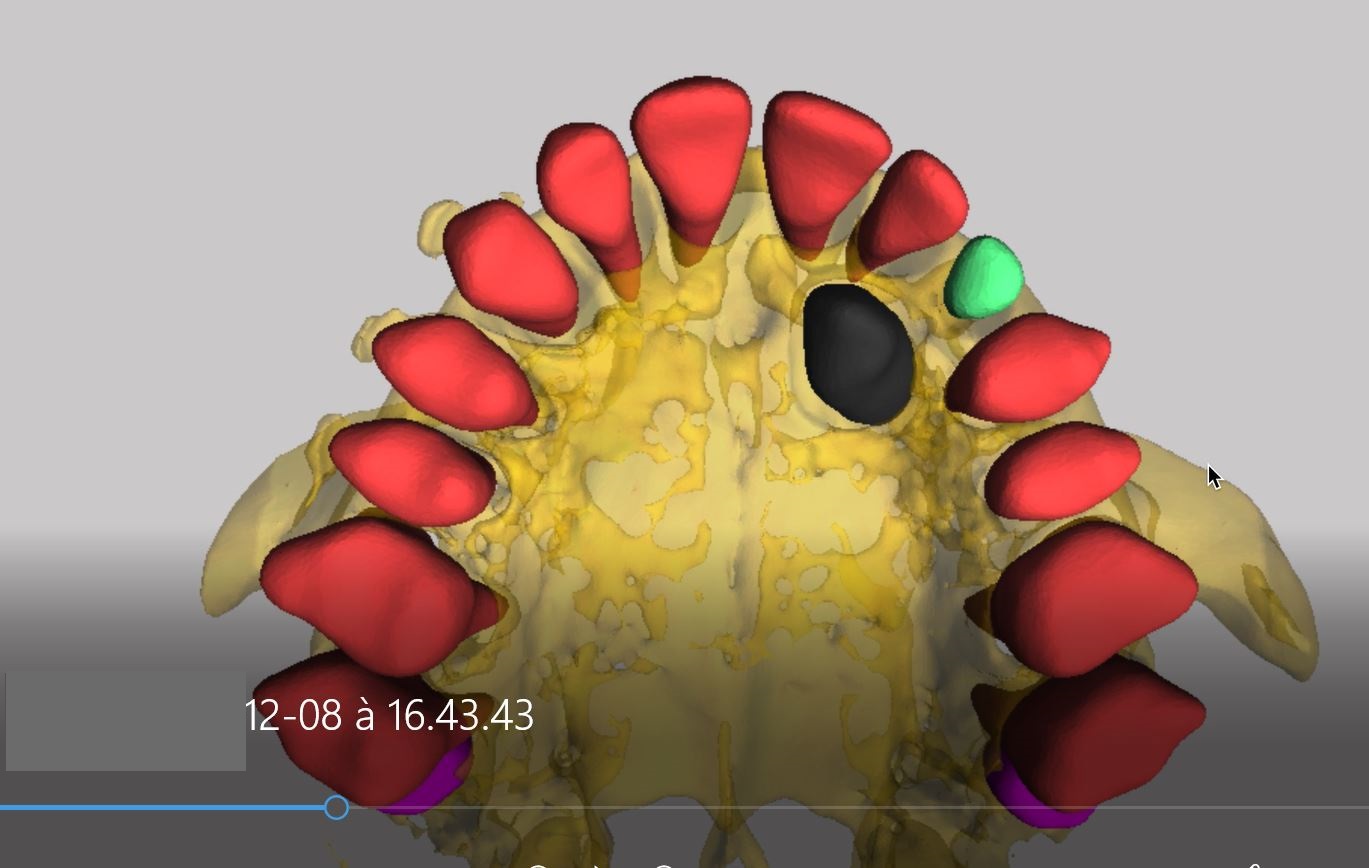
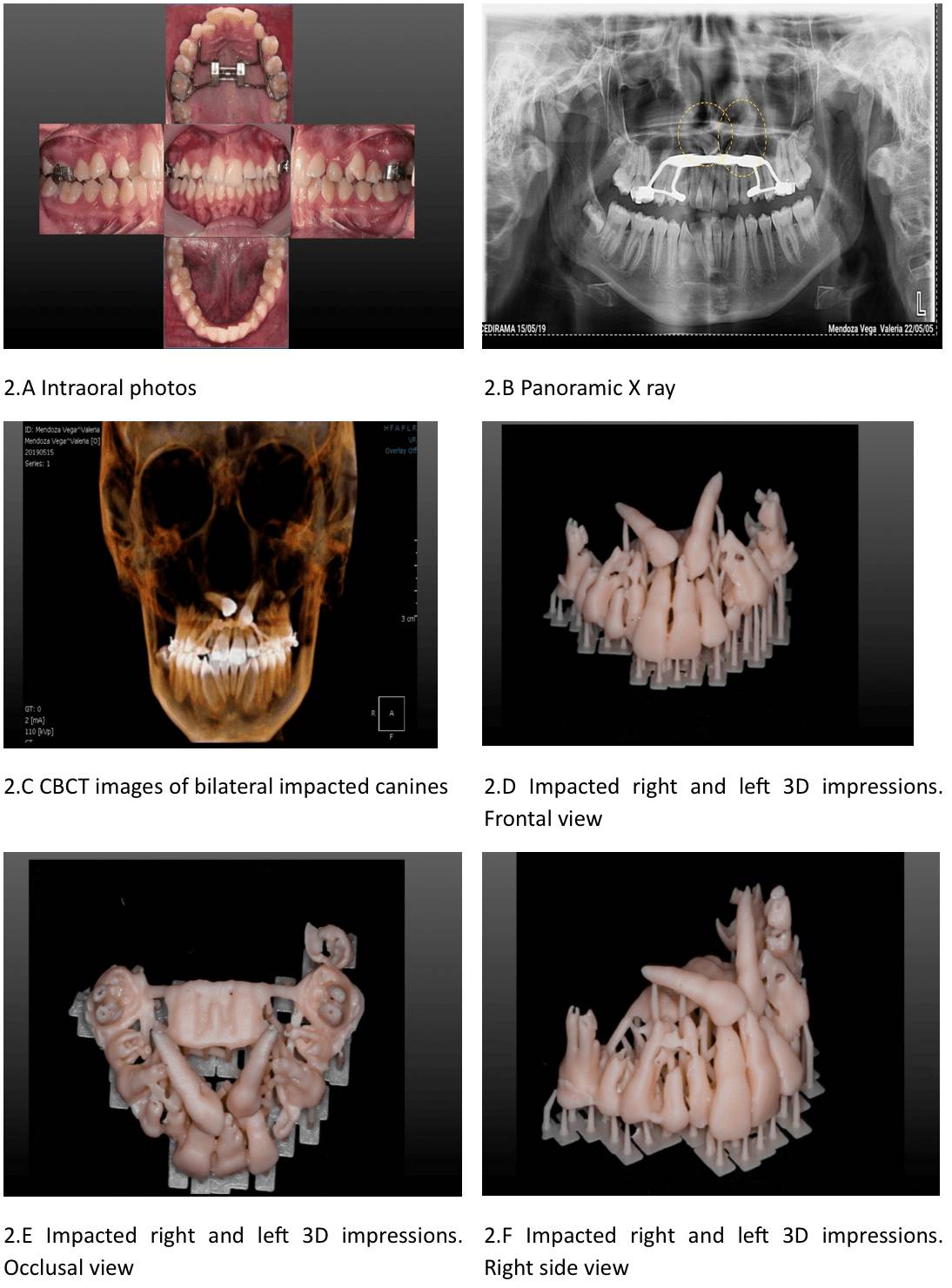
Due to the horizontal position of the right impacted canine, surgical options are clearly the best solution. (Fig.2 a-f).
Conclusions
The use of CBCT in clinical practice can be for a variety of clinical problems, including impacted teeth, craniofacial anomalies, TMJ analysis, and analysis of the upper airway.
Combining CBCT images with 3D segmentations impressions and videos enables a better diagnosis and helps to decide whether to treat these cases orthodontically or surgically.
Special thanks
Orca Dental AI for providing segmentation, video analysis, and cephalometric analysis.
Ideas Dentales Mexico for printing 3D models.
References
- Mason C, Papadakou P, Roberts GJ. The radiographic localization of impacted maxillary canines: a comparison of methods. Eur J Orthod 2001;23:25-34.
- Preda L, La Fianza A, Di Maggio EM, Dore R, Schifino MR, Campani R, et al. The use of spiral computed tomography in the localization of impacted maxillary canines. Dentomaxillofacial Radiol 1997;26:236-41.
- Stewart JA, Heo G, Glover KE, Williamson PC, Lam EW, Major PW. Factors that relate to treatment duration for patients with palatally impacted maxillary canines. Am J Orthod Dentofac Orthop 2001;119:216-25.
- Walker L, Enciso R, Mah J. Three-dimansional localization of maxillary canines with cone-beam computed tomography. Am J Orthod Dentofac Orthop 2005;128:418-23.
- Peck S, Peck L, Kataja M. The palatally displaced canine as a dental anomaly of genetic origin. Angle Orthod. 1994;64:249-56.
- Ericson S, Kurol J. CT diagnosis of ectopically erupting maxillary canines – a case repost. European Juornal fo Orthodontics 1988;10:115-21.